News
Archive for August, 2016
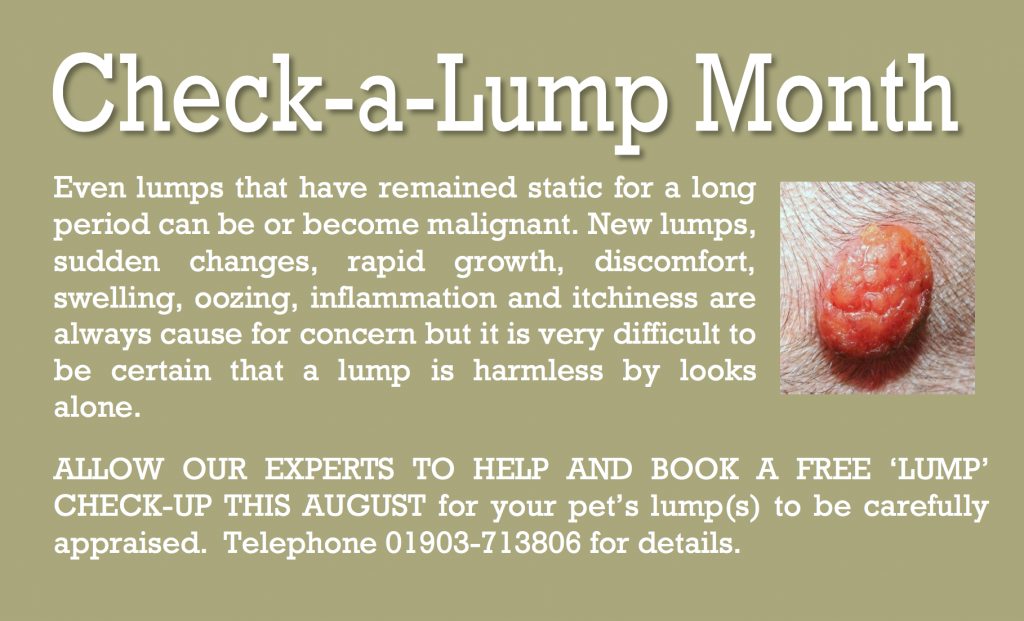
Special Offer: Check a Lump Month
by admin on August 1st, 2016
Category: Special Offers, Tags:
Pet of the Month – August 2016 – Brambie
by admin on August 1st, 2016
Category: Pet of the Month, Tags:
Brambie first visited the practice as a second opinion for recurrent bladder/urination problems. A scan revealed she had bladder stones which had not been picked up by her previous vet.
We surgically removed her bladder stones and are delighted to report that she is doing very well.
For your interest we include further information on bladder stones below.
What are the symptoms of struvite bladder stones?
The symptoms of bladder stones are very similar to the symptoms of an uncomplicated bladder infection or cystitis. The most common signs that a dog has bladder stones are hematuria (blood in the urine) and dysuria (straining to urinate). Hematuria occurs because the stones rub against the bladder wall, irritating and damaging the tissue and causing bleeding. Dysuria may result from inflammation and swelling of the bladder walls or the urethra, from muscle spasms, or due to a physical obstruction to urine flow caused by the presence of the stones. Veterinarians assume that the condition is painful, because people with bladder stones experience pain, and because many clients remark about how much better and more active their dog becomes following surgical removal of bladder stones.
Large stones may act almost like a valve or stopcock, causing an intermittent or partial obstruction at the neck of the bladder, the point where the bladder attaches to the urethra. Small stones may flow with the urine into the urethra where they can become lodged and cause an obstruction. If an obstruction occurs, the bladder cannot be emptied fully; if the obstruction is complete, the dog will be unable to urinate at all. If the obstruction is not relieved, the bladder may rupture. A complete obstruction is potentially life threatening and requires immediate emergency treatment.
My dog has struvite bladder stones. What does that mean?
Dogs, like people, can develop a variety of bladder and kidney stones. Bladder stones (uroliths or cystic calculi), are rock-like formations of minerals that form in the urinary bladder, and are more common than kidney stones in dogs. One of the more common urolith in the dog is composed of magnesium ammonium phosphate hexahydrate. The more common name for this type of bladder stone is “struvite bladder stone”.
How did my dog get them?
Normal dog urine is slightly acidic and contains waste products from metabolism including dissolved mineral salts and other compounds. Struvite is a normal component of dog’s urine and will remain dissolved as long as the urine is acidic and is not too concentrated. If the urine becomes exceptionally concentrated or if it becomes alkaline, struvite crystals will precipitate or fall out of solution.
In dogs, struvite bladder stones usually form as a complication of a bladder infection caused by bacteria that produce an enzyme known as urease. This enzyme breaks down the urea that is normally present in the urine causing an excess production of ammonia; this ammonia production then causes the urine to become alkaline. Ammonia in the urine also causes bladder inflammation. Under these environmental conditions, struvite crystals will precipitate out of solution and collect around any cells or debris that may have formed in the bladder as a result of inflammation. Female dogs tend to get these types of bladder infections and stones much more frequently than males, probably because their shorter, wider urethra makes it easier for bacteria to pass up the urethra into the bladder. In some studies, up to 85% of dogs with struvite bladder stones were female.
Other causes of alkaline urine such as certain kidney diseases, long-term use of diuretic drugs or antacids, and other conditions that cause elevated urine pH or elevated levels of urinary phosphorus or ammonia can also predispose a dog to the formation of struvite bladder stones.
How common are struvite bladder stones?
Bladder stones are somewhat common in dogs, and struvite stones are the most common; in clinical studies, up to 26% of all bladder stones were found to contain struvite. Together, struvite and calcium oxalate uroliths have been found to comprise over 85% of all uroliths submitted for laboratory analysis in a recent study. Based on the results of tens of thousands of stone analyses, it has been found that the number of struvite bladder stones has been declining in dogs while the number of calcium oxalate stones has been increasing during the past ten years. Struvite uroliths were noted to be more common in female dogs and calcium oxalate uroliths in male dogs. Breeds most commonly diagnosed with struvite and calcium oxalate bladder stones included: shih tzu, miniature schnauzer, bichon frisé, lhasa apso, and Yorkshire terrier.
How are struvite bladder stones diagnosed?
In some cases, your veterinarian may be able to palpate (feel) struvite stones in the bladder if the dog is relaxed and the bladder isn’t too painful. However, some stones are too small to be felt this way. Often, bladder stones are diagnosed by means of an x-ray of the bladder, or by means of an ultrasound. Struvite stones are almost always ‘radiodense’, meaning that they can be seen on a plain radiograph. However, sometimes bones or other overlying body parts will interfere with the ability to see bladder stones with regular x-rays, in which case your veterinarian may recommend a contrast study, a specialized technique that uses dye to outline the stones in the bladder, or a bladder ultrasound.
These imaging procedures will identify the presence of a bladder stone, but will not definitively tell your veterinarian the composition of the stone. The only way to be sure that a bladder stone is made of struvite is to have the stone analyzed at a veterinary laboratory.
In some cases, your veterinarian may make an educated guess about the type of stone that is present, based on the radiographic appearance and results of a urinalysis. For example, if x-rays show that there are one or more stones present in the bladder, and the results of the urinalysis show the presence of alkaline urine along with numerous struvite crystals, your veterinarian may make a presumptive diagnosis of struvite bladder stones and recommend treatment accordingly.
How are struvite bladder stones treated?
There are three primary treatment strategies for struvite bladder stones:
1) Feeding a special diet to dissolve the stone(s)
2) Non-surgical removal by urohydropropulsion
3) Surgical removal
1) Feeding a special diet: The use of special therapeutic diets to dissolve struvite bladder stones is often recommended in cases where the risk of a urinary tract obstruction is relatively low. These diets typically are restricted in protein, phosphorus and magnesium and are formulated to promote formation of acidic urine (with a pH less than 6.5). This formulation helps dissolve struvite stones that are already present in the urine, and prevents formation of further stones. Dissolution of the stones is further enhanced by increased water intake, which will serve to dilute the urine.
Since most dogs with struvite bladder stones developed them as a result of a bladder infection, the dog will also be placed on antibiotic therapy while the stones are being dissolved. This is important because, as the layers of stone are dissolved, bacteria that have become trapped in the layers of stone are released into the bladder; if left untreated these bacteria can set up another infection. Some dogs may experience dissolution of struvite stones within two weeks while others may take up to 12 weeks. Your dog will need to have antibiotics during this entire period of time. If your dog is placed on dietary therapy to dissolve the bladder stones, your veterinarian will recommend that a urinalysis and bladder x-rays should be performed approximately every four to six weeks during treatment.
Some bladder stones can be ‘mixed’ or composed of multiple layers of different types of mineral, which may complicate treatment. If follow-up x-rays show that the stones are no longer dissolving, this may indicate that the stones are mixed, and the treatment plan may need to be adjusted.
2) Non-surgical removal: If the bladder stones are very small it may be possible to pass a special catheter into the bladder and then flush the stones out, in a technique called urohydropropulsion. In some cases, this procedure may be performed with the dog under heavy sedation, although general anesthesia is often necessary. If your veterinarian has a cystoscope, small stones in the bladder or urethra can sometimes be removed with this instrument, thus avoiding the need to cut the abdomen and bladder open. Either of these procedures may also be used to obtain a sample stone for analysis so that your veterinarian can determine if dietary dissolution is feasible.
3) Surgical removal: Surgery is indicated in dogs that have a large number of stones in their bladder, if there is an increased risk that the patient will develop an obstruction in the urinary tract, or if the client wishes to have the problem resolved as quickly as possible. Male dogs are at a much higher risk of developing an obstruction in the urinary tract as a result of bladder stones, so when bladder stones are diagnosed in a male dog, your veterinarian will often strongly recommend surgical removal. Surgery is also indicated if dietary treatment was not successful in eliminating the stones, or If it appears that the stones are composed of a mixture of mineral types. Your veterinarian will discuss the appropriate treatment strategy for your dog, based on your individual situation.
Are there any other treatment options?
In some selected referral centers, another option may be available to treat bladder stones. This option is ultrasonic dissolution, a technique in which high frequency ultrasound waves are used to disrupt or break the stones into tiny particles that can then be flushed out of the bladder. It has the advantage of immediate removal of the offending stones without the need for surgery. Your veterinarian will discuss this treatment option with you if it is available in your area.
How can I prevent my dog from developing struvite bladder stones in the future?
Dogs that have experienced struvite bladder stones will often be fed a therapeutic diet for life. Diets lower in protein, phosphorus and magnesium and promote acidic urine are recommended. The preventative diet is NOT the same as the diet that promotes dissolution of the stones. In certain cases, medications to acidify the urine may be required. In addition, careful routine monitoring of the urine to detect any signs of bacterial infection is also recommended. Bladder x-rays and urinalysis will be performed one month after successful treatment, dietary or surgical, and then every three to six months for life. Dogs displaying any clinical signs of urinary tract infections such as frequent urination, urinating in unusual places, painful urination or the presence of blood in the urine should be evaluated immediately. Keep in mind that the greatest risk factor for developing struvite bladder stones in the dog is a urinary tract infection.
Chronic Inflammatory Bowel Disease (IBD) in Dogs
by admin on August 1st, 2016
Category: News, Tags:
Chronic inflammatory enteropathy (or CIE) is a disease that causes inflammation of the bowel. It has some similarities to a human disease called Crohn’s disease. The inflammation can affect any or all of the stomach, small bowel and large bowel (colon).
What are the signs of chronic inflammatory bowel problems in dogs?
Gastrointestinal (bowel) signs are considered chronic when they have been present for three weeks or more and often clinical signs will come and go. The most common signs associated with gastrointestinal tract disease in dogs include vomiting and diarrhoea. It is important to remember that diarrhoea is a term used to describe altered stool frequency as well as altered stool consistency. Blood and mucus are sometimes seen mixed with the stool. Abdominal pain, ‘squeaky’ guts (this is called ‘borborygmi’) and wind can also be seen. Some cats with chronic inflammatory bowel disease will have no vomiting or diarrhoea and their main sign will be reduced appetite.
What causes chronic inflammatory enteropathy in dogs?
The gastrointestinal signs seen in chronic inflammatory enteropathy arise due to inflammation of the wall of the intestines and/or stomach. The initial cause of the inflammation is often unknown; environmental and genetic factors are thought to play a role along with an abnormal response of the body’s immune system that normally fights infection. Chronic inflammatory enteropathy is generally considered to be an ‘idiopathic’ disease (i.e. a disease with no known underlying cause). The diagnosis is one of exclusion and the diagnosis can only be made if other possible causes of the signs have been excluded.
Chronic inflammatory enteropathy is not a single disease process but it is actually a catch-all term applied to a number of diseases with similar signs. It encompasses food responsive disease (FRD), antibiotic responsive diarrhoea (ARD) and inflammatory bowel disease (IBD).
- Food responsive disease is diagnosed when a dog or cat has clinical signs of gastrointestinal tract disease that responds to dietary modification.
- Antibiotic responsive diarrhoea is the term used when gastrointestinal tract signs respond to antibiotic(s) and relapse when antibiotics are stopped. The immune system is thought to have an exaggerated response to ‘normal’ gut bacteria in patients with this disease. It is important to note that antibiotics are not normally indicated in sudden (acute) onset diarrhoea.
- Inflammatory bowel disease has a complex set of underlying causes. It is diagnosed with bowel biopsies that are normally taken with the aid of a camera (endoscope) meaning that surgery is not necessary. It is normally managed with steroid therapy.
Which breeds can be affected by chronic inflammatory enteropathy?
Chronic inflammatory enteropathy can occur in any breed of dog, but certain breeds such as German Shepherds, Soft-coated Wheaten terrier and Irish Setters are known to have an increased risk. It is typically a disease of the middle aged dog but any aged dog can be affected. Cats can also get CIE.
How is chronic inflammatory enteropathy diagnosed?
Chronic inflammatory enteropathy in dogs is normally diagnosed on the basis of history, blood tests, abdominal imaging (typically an ultrasound scan) and sometimes camera evaluation of the upper and/or lower bowel.
How are chronic inflammatory bowel problems in dogs treated?
Dependent upon the severity of the presenting signs, a change in diet may be the first treatment undertaken by your vet. Generally diet trials are performed using a diet that contains a single protein source or one where the proteins are broken down to such a small size (hydrolysed) that they are not recognised as ‘foreign’ by the immune system in the bowel. Some vets prefer to use a single protein source that the patient is unlikely to have been exposed to before (i.e. duck or venison). The diet is normally fed for a minimum of two to four weeks but many dogs respond sooner. If the signs respond to dietary therapy, a diagnosis of food responsive disease is made and dietary therapy is continued long term.
If patients fail to respond to a diet trial or only partially respond, antibiotics may be trialled. If the signs respond, a diagnosis of antibiotic responsive diarrhoea is made.
If the animal’s clinical signs persist despite dietary change or antibiotic therapy, or if the clinical signs are particularly severe, camera examination of the bowel will be performed. This is called endoscopy and the procedure is always done under general anaesthesia in animals. Small biopsies are taken from the bowel during this procedure. Assuming inflammation is identified on the biopsies, a diagnosis of inflammatory bowel disease is made. Inflammatory bowel disease is managed with drugs that suppress the immune system’s exuberant response. A steroid called prednisolone is often the first choice medication in both dogs and cats. Additional medications such as ciclosporin and chlormabucil are sometimes used.
What is the outlook for chronic inflammatory bowel disease in dogs?
The outlook for patients with chronic inflammatory enteropathy is dependent upon the severity of the signs and the response to treatment. Many patients will experience intermittent flare ups of their disease long term despite therapy but these are typically milder and shorter in duration once animals are receiving appropriate treatment. Unfortunately a very small proportion of dogs with IBD have disease that is not responsive to drug therapy.